UNDERSTANDING CLOWARD SIGN
Cloward Sign is likely one of those topics you briefly scanned over in school and haven’t though much about since. An oldie but a goodie, Cloward Sign is a good reminder to always keep your list of differential diagnoses long to avoid bias in your evaluation. That pain along the shoulder blade might present like rhomboid pain but how do you know it’s not C6-7 facet or levator scapula or intervertebral disc (IVD) referral pain? With so many possibilities in this area, it’s important to keep an open mind and perform a thorough evaluation to determine the true source of symptoms. Keep reading to review up on Cloward Sign and learn how I like to structure my evaluations to rule in or out possible diagnoses.
A history of cervical intervertebral disc knowledge
Let’s start out with a history lesson. Prior to 1959 it was widely accepted that neck pain could be caused by 3 general things:
Cervical muscles and ligaments
Intervertebral discs involving the nerve root
Cervical spondlyosis
But at the time it was difficult to isolate the exact anatomical structure involved. IVD pathology was assumed to be due to an encroachment or compression of the surrounding nerve root. There was no evidence that discs themselves could refer pain, despite instances with patients complaining of referred pain without radicular symptoms or neurological involvement. Dr. Cloward’s 1959 study was the first to demonstrate the effect that disc pathology without nerve involvement had on referral patterns.
In a study that would have questionable ethical standards compared to our standards today, Cloward and his team used a local anesthetic on live, awake patients (med students) to then stimulate various parts of the cervical intervertebral disc and monitor their symptoms. Upon stimulating the anterior surface, patients complained of severe pain around the scapular vertebral border on the same side with no pain through the arm. Stimulation of the posterior surface referred to the upper shoulder blade, the base of the neck, the top of the shoulders, the inferior angle of the scapula, and down the posterior arm to the elbow. These pain referral patterns are now termed “Cloward Sign”.
Anterior disc referral patterns
C3/4 disc: C7 spinous process and top of shoulder
C4/5 disc: region of the spine and superior angle of the scapula
C5/6 disc: center oft the scapular border
C6/7 disc: region of the interior angle of the scapula
Posterolateral disc referral patterns
C4/5 disc: pain spreads out from a band from the base of the neck to the top of the shoulder
C5/6 and C6/7 discs: pain over the scapula, across the shoulder joint, and along the lateral or posterior regions of the upper arm to the elbow
Difficulties with differential diagnoses
It is not uncommon for patients complaining of pain in these areas to simultaneously present with muscle spasms in the area which might lead one to assume that treating the area will result in reduction of symptoms. However, the muscle spasm is more likely to be secondary to the source of pain, also known as secondary hyperalgesia. While the skin that lays over the medial scapular border is innervated by T2-T7 spinal nerves, the muscles laying below this region are innervated by the brachial plexus (C5-T1).
Facet joint referral
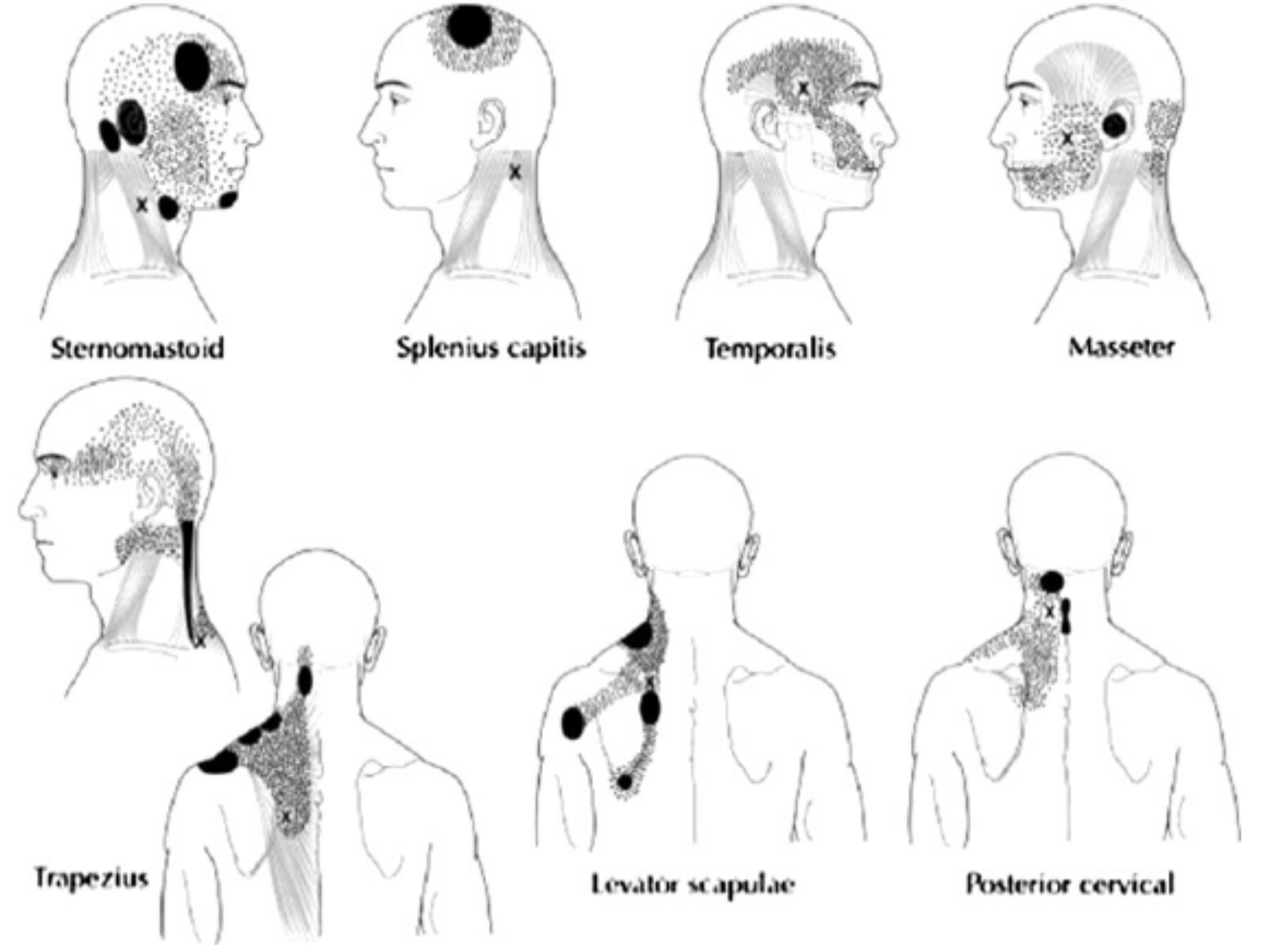
Myofascial trigger point referral
In fact, pain in these areas can also be caused by referral symptoms from the facet joints in addition to trigger points, which both have overlapping presentation patterns. So how do you determine the cause of symptoms? Below is the simplest breakdown of a complex presentation:
Establish the baseline symptoms of your patient, prior to introducing a stimulus. If symptoms are currently present, a very easy way to rule in the Cloward sign is to apply manual cervical traction. This should be completed in sitting and make sure to apply graded (I-III) traction with heightened caution for patients presenting with high severity/irritability. If symptoms reduce, the odds are higher that the pain is being generated from the cervical spine. If symptoms are unresponsive to traction, then I will combine a lateral shift (to the side of pain) and traction to help increase the offloading to the symptomatic side. With no change with the combined traction stimulus, then I will progress to approximation (compression) to increase the load to the cervical spine. Side glide to the ipsilateral side can also be included if non-responsiveness to the compressive force. If symptoms are not aggravated with the approximation stimulus, I feel strongly that the symptoms are not cervicogenic and not an actual Cloward sign.
About the Author: Jess Elis
Jess is the Founder of Rehab Code and brings an extensive experience level in the world of sports and orthopedic PT. He is focused on moving the proverbial "needle" to enhance the PT profession through education and mentorship. Most of this education will be driven through social media/blogs; in hopes to either educate the masses or expose them to his rather odd and eclectic musical taste. Either way, it's a win in his books.
Follow Jess